Professor Tony Marson

This is an archived programme
The North West Coast epilepsy pathway identified an extra 66% of epilepsy-related admissions when compared to just using the primary diagnosis code, now capturing more accurate average length of stay
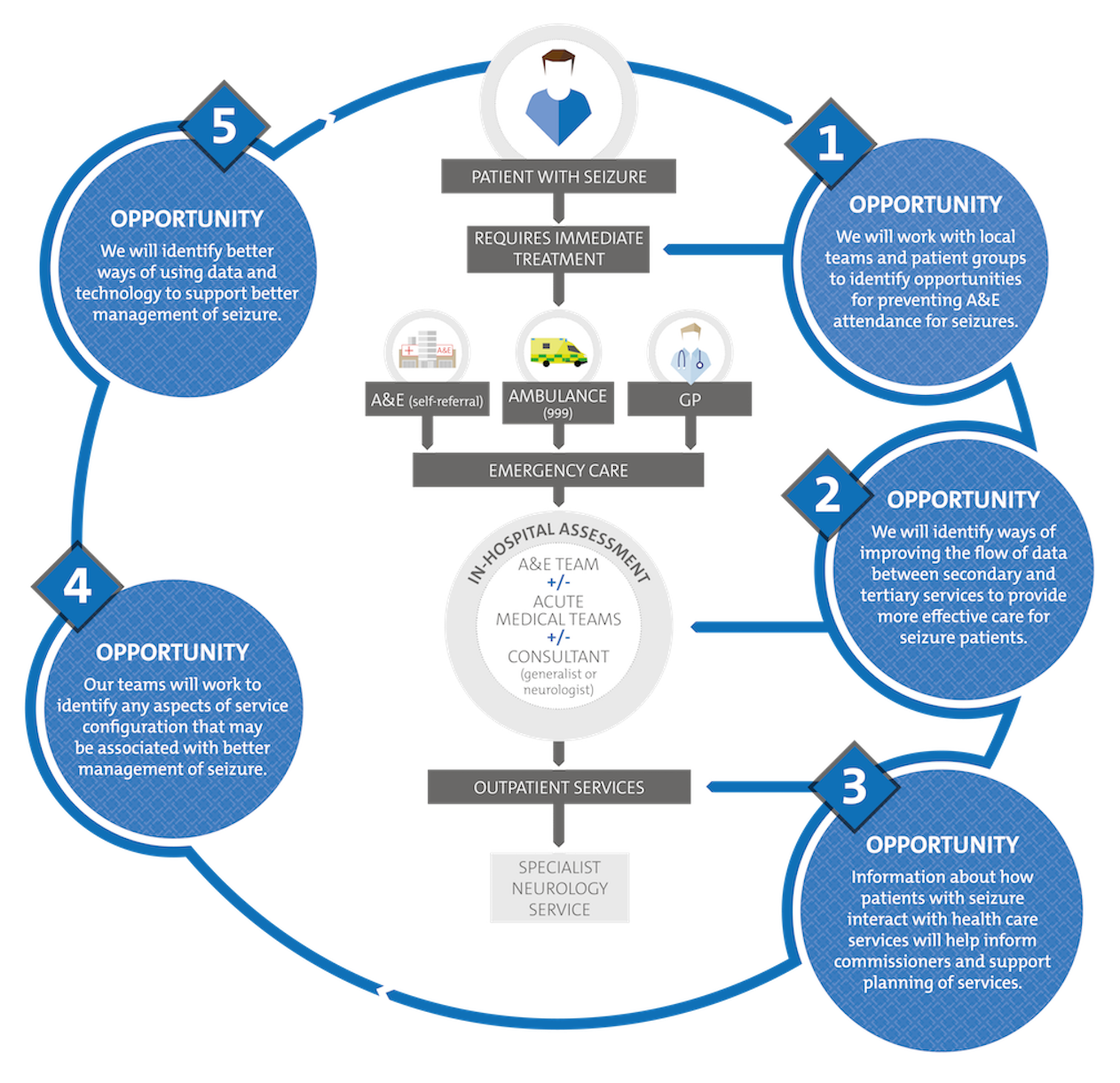
Epilepsy and seizures are the most common neurological reason for emergency presentations at hospital.
They account for 1.5% of emergency admissions and a similar number are discharged from the emergency department without admission.
Many seizure admissions are preventable and improvements in care are needed. NICE guidelines recommend that patients experiencing their first-ever seizure should be seen in a seizure clinic within two weeks but this is rarely the case.
The detection of an extra 40% of cases of ALRD when with standard approaches for capturing data on emergency admissions resulted in improved knowledge of disease burden and better monitoring of inpatient and post-discharge outcomes.
The team at the University of Liverpool used routinely collected hospital data to assess the impact of interventions such as the Walton Seizure Pathway and the Care After Presenting with Seizures (CAPS) Project and monitor the effect of these interventions on health inequalities.
Geographical data was analysed to allow patterns of high admissions rates to be identified and fed back to CCGs within Cheshire and Merseyside; this led to the planning of community-based epilepsy clinics.
Routinely collected hospital data was analysed to identify unnecessary CT scans, highlighting inadequate coordination in care and leadership, wasted resources, and unnecessary exposure of patients to radiation.
Epilepsy pathway impacts
- Analysis of data showed that since the instigation of the Walton Seizure Pathway, the odds of getting a neurology referral within three months of a seizure admission were increased by 28% for those already known to the service, and by 48% for those newly identified. A further increase in the odds was observed for hospitals where nurses were employed part-time to facilitate referrals (by 105% for newly identified cases).
- South Sefton CCG used geographical data relating to the source of epilepsy admissions to plan community-based epilepsy clinics, run in a local GP surgery by a Walton Centre neurologist.
- Adoption of the NWC CHC algorithm at a national level including by the National Neurology Advisory Group (NNAG) and the NHSE Epilepsy Specialist Commissioning Review.
- The Getting It Right First Time (GIRFT) neurology group gained insights from the work undertaken by the CHC NWC team on using routine data to identify admissions and calculate referral rates and now uses the three-month referral rate as a key metric on which to measure hospital performance.
- The epilepsy pathway work also led to the PED4PED Project funded by MRC/HDRUK which aims to provide paramedics with access to epilepsy care records from secondary care in order to inform decisions about conveyance and immediate care.
Continue reading: Impacting on care for alcohol-related illness >

